
The use of vitreous humor (VH) in forensic casework has been growing in the last years due to numerous advantages. This review includes resources for pharmacists, patients, and caregivers reviews currently available treatments and discusses seizure action plans that support effective treatment of seizure clusters.
#Rectal diazepam antidote how to#
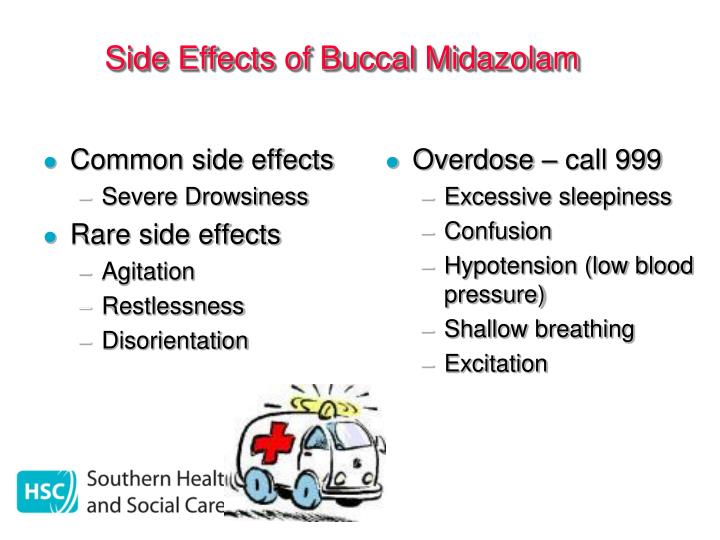
Pharmacists' counseling plays an important role in reinforcing when and how to appropriately administer rescue therapies and the importance of consistently using rescue treatment when indicated to promote effective management. Recognition of seizure clusters and timing of proper administration are key to successful use of rescue therapy.
Both offer a convenient and socially acceptable route of administration. Each of the approved intranasal formulations has a unique profile. In the 2 decades before the approval of 2 intranasal benzodiazepines in 20, rectal diazepam was the only route of administration approved by the US Food and Drug Administration specifically for seizure clusters. The ideal rescue therapy allows for easy and quick administration by a nonmedical person, which may minimize the need for intervention by emergency medical personnel or transportation to the hospital.

Most seizure clusters occur outside the hospital setting. Prompt, appropriate use should be specified in patients' individualized seizure action plans. Rescue therapy is based on benzodiazepine treatment. Left untreated, seizure clusters increase the risk for physical injury and may progress to status epilepticus, irreversible neurologic injury, and death. Some patients with epilepsy experience seizure clusters, which may be defined as 2 or more seizures occurring within 24 hours. "Autophagy checkpoint inhibition" (ACI) can be achieved by targeting DBI/ACBP. We conclude that a-DBI-mediated neutralization of extracellular DBI/ACBP mediates potent autophagy-dependent organ protection by on-target effects, hence unravelling a novel and potentially useful strategy for autophagy enhancement. The hepatoprotective effects of a-DBI against MCD are mimicked by three alternative strategies to block DBI/ACBP signaling, in particular (i) induction of DBI/ACBP-specific autoantibodies, (ii) tamoxifen-inducible knockout of the Dbi gene, and (iii) a point mutation in Gabrg2 (gamma-aminobutyric acid (GABA) A receptor, subunit gamma 2 Gabrg2F77I) that abolishes binding of DBI/ACBP. In all these models of organ damage, a-DBI prevents cell loss, inflammation and fibrosis through pathways that are blocked by pharmacological or genetic inhibition of autophagy. We characterized a monoclonal antibody neutralizing mouse DBI/ACBP (a-DBI) for its cytoprotective effects on several organs (heart, liver and lung) that were damaged by surgical procedures (ligation of coronary and hepatic arteries or bile duct ligation), a variety of different toxins (acetaminophen, bleomycin, carbon tetrachloride or concanavalin A) or a methionine/choline-deficient diet (MCD).
DBI/ACBP (diazepam binding inhibitor, also known as acyl coenzyme A binding protein), acts as a paracrine inhibitor of macroautophagy/autophagy.


 0 kommentar(er)
0 kommentar(er)
